The NWT OHT strives to deliver coordinated care through identifying and understanding the needs of our community. To accomplish this goal, our OHT has a number of key priorities, please see below.
Best Practice Spotlight Organizations
The Best Practice Spotlight Organization (BPSO) designation was launched as a key knowledge translation strategy in 2003. It is targeted to support the uptake and sustainability of best practice guidelines (BPG) to optimize outcomes at the individual, organizational and health system levels.
BPSOs have been established across the North Western Toronto (NWT) Ontario Health Team (OHT) partner organization and throughout the world in all sectors. The Ministry of Health designated the Registered Nurses’ Association of Ontario (RNAO) to support organizations within OHTs to implement four Best Practice Guidelines (BPG), over a 4-year period, to support in qualifying for the BPSO designation. This designation is grounded in evidence-based practices. The goal is to create evidence-based practice cultures through systematic implementation and evaluation of multiple RNAO clinical BPGs leading to improved health outcomes.
The BPSO model for Ontario Health Teams was established to respond to health system transformation in Ontario. The model helps OHTs advance all four pillars of the Quadruple Aim as well as the United Nations Sustainable Development Goals (see Figure 1).
The BPSO model focuses its efforts on uptake of best practices across all sectors of the OHT ensuring spread and scale into cultures of excellence. Results are closely monitored and continuous learning is facilitated by coaches to ensure success and sustainability of achievements.
Figure 1: The Quadruple Aim together with the Sustainable Development Goals.
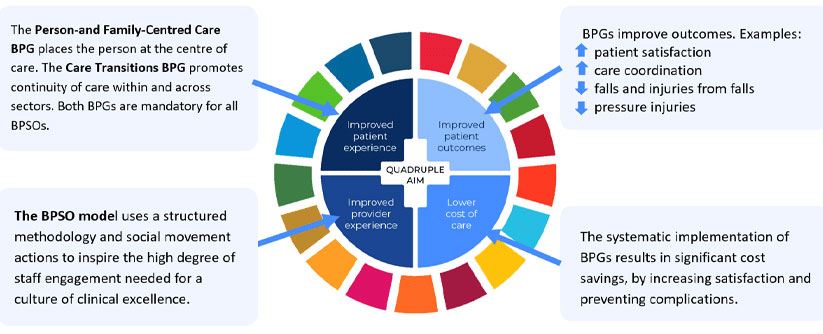
The BPSO program supports the above framework which incorporates the United Nations Sustainable Development Goals (SDGs) (outer circle) together with the Quadruple Aim, addressing population health, supporting underserviced populations and promoting health equity.
Source: Registered Nurses’ Association of Ontario (RNAO), February, 2021, Nurse Practitioner Task Force Report: Vision for Tomorrow.
The Best Practice Champions Network was established in 2002. It consists of thousands of nurses and other health providers, within Ontario and globally, in all roles and health sectors, who are passionate about evidence-based practice and improving care and health. These champions are dedicated practitioners who raise awareness of BPG’s, understand change management processes, motivate their colleagues, and influence the uptake of BPGs among workplace peers. Each participant in the NWT OHT BPSO working group is a champion representative from their organization.
Chronic Obstructive Pulmonary Disease
When looking at areas of focus, the North Western Toronto Ontario Health Team identified COPD as a year one priority population due to the high burden of COPD within North West Toronto. To support this work we created a COPD Working Group.
Chronic obstructive pulmonary disease (COPD) is a lung disease that causes breathing problems. COPD usually develops from chronic irritation and inflammation in your lungs. Obstructive means airflow is blocked, limiting airflow out of your lungs. A COPD exacerbation is when your symptoms suddenly get worse and can become life threatening. They can be triggered by a cold, or flu, or irritants like smoke, fumes, or dust.
The goal of this working group is to:
- Integrate services across care settings to support those who have chronic obstructive pulmonary disease
- Improve how healthcare professionals work together
To address the high burden of COPD within our community, the NWT OHT is working towards developing an integrated collaborative care model (CCM) for COPD, which will include a pathway that reflects the integration of care across different settings such as acute care, community health centers, rehabilitation and home settings. This also involves integrating primary and specialist care as well as the community inter-professional team.
The NWT OHT COPD Pathway is a collaborative care model designed to support patients, families and health care providers in navigating Ontario’s health care system as well as providing avenues to access resources in the community. The objective is to reduce COPD exacerbations and emergency visits, or hospital admissions by connecting a patient to their Care Team via a Care Manager throughout transitions in the health care system.
Community Engagement
Community engagement is critical to the North Western Toronto Ontario Health Team. Going hand-in-hand with the PFAC Partnership and Engagement Strategy, the NWT OHT has a variety of community engagement opportunities:
Recruitment of Community Group
Our OHT aims to recruit for a larger pool of advisors to help engage with on various NWT OHT initiatives.
Community Events
The NWT OHT will host events to bring awareness to the work we do, our partners and educating the community on health services and programs available.
Online Engagement Platform
At maturity, the NWT OHT will be using an online engagement platform to help with managing and evaluating our current community engagement initiatives.
Digital Health
The world is going (or should we say, has gone) digital. The North Western Toronto Ontario Health Team formed the Digital Health Committee to oversee all matters related to information management, privacy, and other digital health initiatives across the NWT OHT.
Digital health technology aims to improve our health and wellbeing, and to improve health systems. It includes smartphone apps, wearable devices (such as step trackers), and platforms that provide remote healthcare (telehealth). Software to help track symptoms, online tools to diagnose conditions, and programs that analyze data from medical devices such as blood pressure monitors – these are all digital health technologies.
The goal of this committee is to provide support to our priority populations and health care providers with:
- Accessing virtual care services
- Digital health information
- Online appointment booking through primary care
The NWT OHT is developing a Digital Equity Framework to ensure that digital projects and initiatives are centered in promoting greater digital health equity.
Currently the committee is focused on the following initiatives:
- Online Appointment Booking: Provides patients/clients and caregivers with the ability to book appointments with their primary care providers online, at their convenience.
- Clinical Systems Renewal: Provides primary care providers the opportunity to upgrade their electronic medical record to increase connectivity and efficiency within the system.
- Digital Equity Framework: We are actively working with Ontario Health regions to identify gaps in digital equity and develop a framework to ensure that digital solutions created or planned are equitable and unbiased.
- Patient Navigation: Once again collaborating with our Ontario Health regional partners to develop a common approach for navigation services for our patients.
Health Equity
Since the formation of The North Western Toronto Ontario Health Team, one of our priorities has been to understand the barriers our community faces in relation to access to healthcare. Health equity is imperative to the work of the North Western Toronto Ontario Health. In 2019, our OHT formed a Health Equity Committee comprised of professionals advancing equity, anti-racism and anti-oppression work within the partner organizations which include staff and people with lived experience.
Improving health and health care worldwide requires a focus on equity — equity of access, treatments, and outcomes. Health equity is realized when each individual has a fair opportunity to achieve their full health potential.
This Committee’s purpose is to advance health equity on a system-level across the OHT through the development and implementation of a health equity strategy. The committee has been working on developing a health equity strategy that will inform and guide health equity work in the OHT and in the community.
There are a number of ongoing projects and key milestones that have been achieved out of the committee:
- Committee members have undergone anti-racism and anti-oppression training to help inform their work.
- The NWT OHT have been selected as early implementers of the Engagement, Governance, Access, and Protection (EGAP) framework – a data governance framework for health data from Black communities.
- The NWT OHT have also been selected to participate in the Institute for Healthcare Improvement’s (IHI) Pursuing Equity Learning Network – an 18-month initiative supporting organizations to engage in systems change work.
- We are working with a public health consultancy to support implementation of the EGAP framework and build a Digital Equity Framework that will tie into our Health Equity Strategy.
- We have also conducted a number of focus groups within the community to ensure that our Health Equity Strategy is community-informed.
Mental Health and Addictions
Mental health and addictions (MH&A) is a clinical priority for the North Western Toronto Ontario Health Team. Our community has a higher incidence of mental health and addiction which highlights the importance of this work.
NWT OHT has begun work in three different MH&A areas:
In the fall of 2020, the North Western Toronto Ontario Health Team focused on decreasing the number of hospital admissions for patients with a psychotic disorder. The NWT OHT developed an in-reach community mental health service where community providers, situated in the mental health and addictions inpatient unit at Humber River Hospital, participated in clinical rounds for the early identification and engagement of patients with a psychotic diagnosis.
By having community providers within the hospital, it provides short-term care coordination for patients and allows for better integration with long-term community mental health supports. Implementing this new model of care has led to the NWT OHT patient population experiencing smoother and quicker access to community mental health services once they leave the hospital.
In January 2022, the success of the program led to expansion, including individuals diagnosed with a mood disorder who also experience repeat hospital inpatient admissions. Results from this program will be available when the data has been collected and analyzed.
The North Western Toronto Ontario Health Team has been working to improve services for individuals with substance use disorder who also have repeat visits to the emergency department. In collaboration with the NWT OHT, partners who provide the community with mental health and addiction services, a working group was established.
Based on 2021-22 fiscal year data from Humber River Hospital it was found that:
- People who visit the emergency department (ED) with a substance use disorder were more likely to be male (75%).
- Usually arrive via ambulance.
- The highest number of ED visits took place between 3PM-8PM.
- Alcohol was the common substance (77%), followed by multiple drug use and use of psychoactive substances (8%).
- Individuals who had substance use, mental health and other presenting issues had the highest number of average visits versus those with substance use alone.
Using the data highlighted above, and insights from providers and patient focus groups, the working group has developed initiatives to improve services in the NWT OHT for those who have substance use issues and frequently visit the emergency department. Further details on implementation of these changes will be reported on as they develop.
The Toronto Mental Health and Addictions Access Point (TAP), the centralized MH&A access service in Toronto reported that there has been a nearly three-fold increase in the number of people prioritized (on their waitlist) for intensive case management services in the Northwest sub-region since March 2020. Increases to the waitlist were seen across all areas of Toronto however, North Western Toronto saw one of the largest jumps. This waitlist became the focus of a quality improvement initiative for the OHT. All the OHTs in the province are asked to work on a Collaborative Quality Improvement Plan (cQIP) each year. One area of focus for each OHT is in the MH&A area and the goal is to work on a project which will help the community get better access to MH&A services. So, the NWT OHT decided to work on ways to reduce the TAP waitlist for their cQIP project for the 2021-22 year.
A workgroup was setup to explore the reasons why people are waiting for access to intensive case management. OHT partners in the workgroup included Across Boundaries, Canadian Mental Health Association – Toronto Branch and Cota Health. The workgroup developed 14 new services/service innovations which will help to decease the wait time for intensive case management services. From June to August 2022, nearly 10 of the service innovations have been implemented across the various MH&A partner organizations and this has resulted in reducing the wait-time to care.
Primary Care
Primary care is crucial to integrated care and advancing the goals of the Ontario Health Team. In the NWT OHT, 11% to 20% of the community do not have access to a primary care provider. The NWT OHT has a Physicians Association Executive Committee. This Committee is responsible for leading the strategic direction for primary care in the OHT.
The Committee is comprised of leadership from the following primary care practices which represent 174 physicians:
- Humber River Family Health Organization and Family Health Team
- Finch Weston Health Centre
- Yorkview Medical Centre
- North Western Toronto Family Health Group
- Jane and Finch Family Health Teama
- Marlee Medical Family Health Group
* Data from 2020: Ministry of Health Data Package
Data from the Ontario Medical Association indicates there are 244 practicing primary care physicians in north western Toronto, with 41% of them being later on in their career (Aug 1, 2022, OMA).
The percentage of our local population enrolled to a Family Health Team is 12.2% compared to the provincial average of 23.3%.
Approximately 3% of people receive their primary care from a doctor at a Community Health Clinic.*
26% of the population have 2-4 primary care visits per year, while 52% have 5 or more visits per year.*
This Committee’s purpose is to embed the perspective of primary care throughout OHT initiatives and activities. Additionally, to create a learning environment to spread and scale best practices across the network.
There are a number of ongoing projects and activities that include but are not limited to:
- Improving cancer screening rates
- Expanding membership and recruiting more primary care leaders
- COVID-19 Recovery Initiatives